Diabetic Neuropathy – Causes, Symptoms, Diagnosis & Advanced Treatment
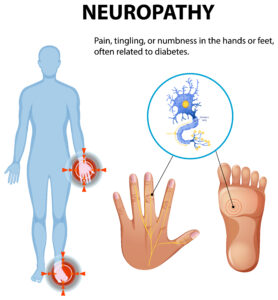
What Is Diabetic Neuropathy?
Diabetic neuropathy is a condition where nerves become damaged due to long-standing elevated blood glucose levels. This nerve damage affects:
- Sensation (sensory nerves)
- Muscle movement (motor nerves)
- Sweating and circulation (autonomic nerves)
Over time, patients may experience:
- Numbness
- Tingling
- Burning pain
- Loss of feeling
- Foot injuries without pain
- Balance problems
If not treated early, neuropathy can lead to ulcers, deformities, falls, and infections.
Causes of Diabetic Neuropathy
Diabetic neuropathy is caused by a combination of metabolic and vascular factors:
1. Uncontrolled Blood Sugar
High glucose levels damage nerves and reduce their ability to transmit signals.
2. Reduced Blood Supply to Nerves
Diabetes affects small blood vessels supplying nerves, leading to nerve ischemia and degeneration.
3. Metabolic Dysfunction
High blood sugar produces toxic byproducts:
- Sorbitol
- Advanced glycation end-products (AGEs)
These damage nerve fibers.
4. Inflammation
Chronic inflammation in diabetics contributes to nerve injury.
5. Lifestyle Factors
- Obesity
- Smoking
- High cholesterol
- Alcohol use
increase the risk and severity of neuropathy.
Pathology of Diabetic Neuropathy (What Happens Inside the Body?)
Diabetic neuropathy involves multiple pathological changes:
1. Nerve Fiber Degeneration
- Loss of myelin (protective nerve covering)
- Axon damage (nerve fiber injury)
- Slowed nerve conduction
2. Microvascular Damage
Blood vessels supplying nerves become narrowed, reducing oxygen delivery.
3. Accumulation of Toxic Metabolites
High glucose leads to the buildup of sorbitol and fructose inside nerves, causing swelling and dysfunction.
4. Oxidative Stress
Free radicals damage nerve cells and worsen neuropathy.
5. Loss of Protective Sensation (LOPS)
Nerve degeneration leads to:
- Numbness
- Painless injuries
- Increased ulcer risk
Diabetic Neuropathy symptoms
Symptoms vary depending on the severity and type of nerve damage. They may develop gradually or worsen suddenly.
Common Symptoms:
- Numbness or reduced ability to feel pain
- Tingling or “pins and needles” sensation
- Burning or stabbing pain
- Sharp electric-shock–like pain
- Increased sensitivity to touch (hyperesthesia)
- Muscle weakness or cramps
- Loss of balance
- Dry or cracked feet due to reduced sweating
- Deformities like hammer toe, claw toe
- Ulcers due to unnoticed injuries
Advanced Symptoms:
- Complete loss of sensation
- Charcot foot (bone & joint destruction)
- Frequent falls
- Serious foot infections
Diagnostic Tests for Diabetic Neuropathy
A thorough evaluation helps detect neuropathy early and prevent complications.
1. Clinical Examination
- Sensory test for touch, pain & temperature
- Muscle strength testing
- Balance assessment
- Checking for calluses, cracks, or ulcers
2. Monofilament Test
A simple test using a nylon filament to check loss of protective sensation.
3. Vibration Test (128 Hz Tuning Fork)
Assesses vibration sensation at the big toe and ankle.
4. Nerve Conduction Studies (NCS) / Electromyography (EMG)
Measures how fast nerves carry signals; helpful in advanced cases.
5. Biothesiometry
Quantifies vibration perception threshold.
6. Reflex Testing
Achilles tendon reflex helps detect early neuropathy.
7. Foot Pressure Scan
Identifies high-pressure areas that can lead to ulcers.
8. Blood Tests
To evaluate:
- Blood sugar levels
- HbA1c
- Vitamin B12
- Thyroid function
Diabetic Neuropathy treatment
Neuropathy cannot be reversed completely, but with proper treatment, symptoms can be controlled, nerve damage progression slowed, and complications prevented.
1. Blood Sugar Management
Strict glucose control is the most important step in neuropathy treatment.
- Lifestyle modification
- Diet & exercise
- Oral medications or insulin
- HbA1c monitoring
2. Medications for Nerve Pain
Neuropathic pain can be controlled with:
- Pregabalin
- Gabapentin
- Duloxetine
- Amitriptyline
- Alpha-lipoic acid
These reduce burning, tingling, and shooting pain.
3. Vitamin Therapy
Deficiencies can worsen neuropathy. Supplements include:
- Vitamin B12
- Vitamin B6
- Vitamin D
- Antioxidants
4. Advanced Foot Care & Ulcer Prevention
- Daily foot inspection
- Nail and callus care
- Moisturizing dry feet
- Avoiding barefoot walking
- Treatment of minor injuries
5. Offloading & Orthotics
Custom footwear reduces pressure on sensitive areas to prevent ulcers:
- Diabetic shoes
- Insoles
- Custom orthotics
- Offloading boots
6. Physiotherapy & Rehabilitation
Improves muscle strength and balance:
- Nerve stimulation therapies
- Stretching & strengthening exercises
7. Wound Care for Neuropathy-Linked Ulcers
If neuropathy causes ulcers:
- Regular debridement
- VAC dressing
- Advanced wound care
- Infection management
- Surgical correction if needed
8. Lifestyle Changes
- Quit smoking
- Reduce alcohol
- Maintain healthy weight
- Manage cholesterol
These improve nerve health and blood flow.
