Foot Swelling, Heel Pain & Plantar Fasciitis in Diabetic Patients – Causes, Symptoms, Diagnosis & Treatment

Foot Swelling in Diabetics
Introduction
Foot swelling (oedema) is common in diabetic patients and may indicate circulation problems, infection, nerve damage, or kidney disease. Persistent swelling can increase pressure on the skin and lead to ulcers, blisters, and difficulty walking.
Causes
Foot swelling in diabetics may result from:
Poor Blood Circulation due to
- Peripheral artery disease (PAD)
- Venous insufficiency
- Diabetic microvascular changes
Infection & Inflammation conditions like
- Cellulitis
- Diabetic foot ulcer infection
- Charcot foot
Neuropathy
It results in weakness in foot muscles which alters gait leading to swelling due to abnormal pressure.
Kidney or Heart Problems
Fluid retention is a common complication in long-standing diabetes leading to chronic kidney disease or ischemic heart disease.
Trauma & Overuse
Injuries, sprains, and repetitive strain can cause localized swelling.
Pathology
Swelling occurs due to leakage of fluid into tissues, poor venous return, inflammatory response, bone/joint instability in Charcot foot and lymphatic obstruction.
Chronic oedema increases the risk of skin breakdown, ulcer formation, infection and reduced circulation
Symptoms
- Puffiness of foot/ankle
- Tightness in skin
- Difficulty wearing shoes
- Redness or warmth
- Heaviness in legs
- Pain or numbness
Investigation
To find the underlying cause, the following tests may be recommended:
- Complete blood count (infection)
- Blood sugar & HbA1c levels
- Kidney function tests (KFT)
- Doppler Ultrasound (arterial/venous circulation)
- X-ray (suspecting Charcot foot)
- MRI (for inflammation or Charcot changes)
Treatment
Treatment depends on the underlying cause:
Medical Management
- Control diabetes
- Treat infection with antibiotics
- Reduce inflammation
- Manage kidney/heart problems
Compression Therapy
If there is no peripheral artery disease then patient should use Diabetic-safe compression stockings.
Elevation & Rest
The patient should keep the feet elevated and avoid prolonged standing.
Offloading in Charcot Foot
Patient is advised either Total Contact Cast or Orthotic boots to stop inflammation, prevent bone destruction, and avoid the characteristic Rocker-bottom deformity, with early initiation (even in stage 0) significantly improving outcomes and shortening treatment time.
Physiotherapy
Physiotherapy for diabetic foot swelling focuses on improving circulation and reducing fluid build up through ankle/foot exercises (circles, wiggles, flex/point), elevation, and regular light movement (walking, swimming) to prevent pooling.
Footwear Modification
Footwear modifications for swollen diabetic feet aim to reduce pressure, accommodate volume changes, and prevent ulceration by using extra-depth, adjustable closures, and specialized, removable, cushioned insoles.
Early care prevents progression to ulcers, gangrene, and deformity.
Heel Pain & Plantar Fasciitis in Diabetics
Introduction
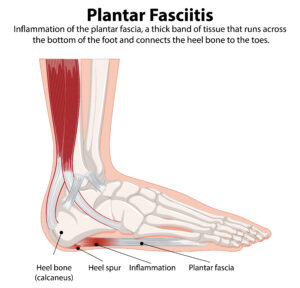
Heel pain is one of the most common foot complaints in diabetic patients. The most frequent cause is Plantar Fasciitis, an inflammation of the plantar fascia, the thick band of tissue connecting the heel to the toes.
Diabetics are more prone to plantar fasciitis due to
- Neuropathy
- Increased foot pressure
- Obesity
- Poor footwear
- Inflammation
Causes
Heel pain and plantar fasciitis may be caused by
- Repeated Stress on Heel can occur due to excess walking, standing, or impact.
- Tight Achilles Tendon
It is common in patients with diabetic neuropathy.
- Improper Footwear
In diabetic patients who wear hard soles, flat footwear, non-supportive shoes are prone for plantar fasciitis.
- Overpronation or Flat Feet
This causes extra strain on plantar fascia.
- Neuropathy-Induced Pressure Changes
It causes loss of protective sensation and motor dysfunction, resulting in elevated, abnormal, and sustained plantar pressures. These high-pressure areas are a critical precursor to foot ulcers and subsequent amputations.
- Obesity
Obesity and diabetes often combine to cause heel pain, primarily from Plantar Fasciitis, worsened by extra weight stressing the fascia, while diabetes stiffens tissue, impairs circulation, and can cause nerve issues, creating a painful cycle.
Pathology
Plantar fasciitis results from
- Micro-tears in the plantar fascia
- Chronic inflammation
- Calcaneal spur formation (heel spur)
In diabetic patients
- Healing is slower
- Inflammation lasts longer
- Pressure points increase risk of ulcer over heel
Symptoms
- Sharp pain at the bottom of the heel
- Pain worse in the morning (“first-step pain”)
- Pain after prolonged standing or walking
- Tenderness over heel
- Stiffness in arch
- Heel swelling
Investigation
- Clinical foot examination
- X-ray (to detect heel spur)
- Ultrasound (plantar fascia thickness)
- Foot pressure scan (identifies pressure overload areas)
- Neuropathy assessment (monofilament test, VPT)
Treatment of Heel Pain & Plantar Fasciitis in Diabetics
1.Medical Treatment
- Anti-inflammatory medications to reduce the inflammation
- Local steroid injections should be given carefully in diabetics
- Neuropathic pain medications if there is nerve involvement
2.Physiotherapy
- Stretching exercises for plantar fascia
- Achilles tendon stretching
- Strengthening foot/ankle muscles
- Ice therapy
- Ultrasonic therapy
3.Footwear & Insoles
- Soft cushioned diabetic footwear
- Heel pads or silicone cushions
- Arch support insoles
- Custom orthotics to improve alignment and reduces pressure
4.Offloading
It reduces pressure on heel with total contact insoles and walking boots in severe cases.
5.Shockwave Therapy (ESWT)
This will help in reducing inflammation & promotes healing in chronic cases.
6.Surgical Treatment
It is rarely indicated only if pain persists > 6–12 months or conservative management fails.
Surgery options like Plantar fascia release or Heel spur removal can be considered depending on patients need.
