What Is Peripheral Artery Disease in Diabetics?
What Is Peripheral Artery Disease in Diabetics?
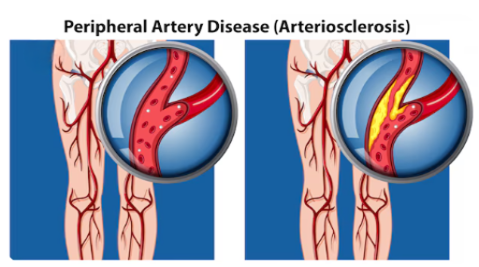
Peripheral Artery Disease (PAD) is caused by atherosclerosis, where plaque builds up inside the arteries. In diabetic patients, the blood vessels become stiff, narrow, and clogged, reducing oxygen delivery to the legs and feet.
This poor circulation leads to:
- Foot ulcers
- Chronic non-healing wounds
- Severe infections
- Gangrene
PAD often remains silent, and many diabetic patients do not notice symptoms until the condition becomes severe.
Early diagnosis is essential to prevent complications and save the limb.
Causes & Risk Factors of PAD in Diabetics
PAD develops due to a combination of metabolic, vascular, and lifestyle factors.
1. Long standing Diabetes
2. Atherosclerosis (Hardening & Narrowing of Arteries)
3. Smoking
4. High Blood Pressure
5. High Cholesterol & Triglycerides
6. Obesity & Sedentary Lifestyle worsens insulin resistance and vascular damage.
7. Age Above 50 years
8. Kidney Disease
Pathology: What Happens Inside the Blood Vessels?
Peripheral artery disease in diabetics involves progressive vascular damage:
1. Endothelial Dysfunction
High glucose levels damage the blood vessel lining, making arteries stiff and prone to injury.
2. Atherosclerotic Plaque Formation
Fat, cholesterol, calcium, and inflammatory cells accumulate inside the artery wall, forming plaques.
3. Artery Narrowing (Stenosis)
The lumen becomes smaller, reducing blood flow to legs and feet.
4. Complete Artery Blockage (Occlusion)
Severe cases result in total obstruction, causing critical ischemia.
5. Reduced Oxygen Supply
Muscles and tissues do not receive enough oxygen, resulting in pain while walking, non-healing ulcers and tissue death (gangrene)
This explains why PAD is one of the biggest causes of delayed wound healing in diabetics
Symptoms of PAD in Diabetics
Symptoms may be mild or absent until PAD becomes severe.
Common Symptoms:
- Leg pain or cramps while walking (claudication)
- Burning pain in feet while resting
- Cold feet or legs
- Numbness or tingling
- Weak or absent pulses
- Slow-healing wounds or ulcers
- Discoloration of toes or foot
- Shiny, thin, or dry skin
Advanced Symptoms (Critical Limb Ischemia):
- Rest pain (severe night pain)
- Gangrene
- Blackened toes
- Deep non-healing ulcers
Investigations / Diagnostic Tests for PAD in Diabetics
Early diagnosis helps prevent ulcers, infection, and amputation.
1. Clinical Examination
- Checking pulses of foot arteries
- Skin temperature
- Capillary refill
- Ulcers or color changes
2. Ankle–Brachial Index (ABI)
A simple test comparing ankle and arm blood pressure.
ABI < 0.9 indicates PAD.
3. Doppler Ultrasound Scan
4. Toe Pressure / TBI (Toe-Brachial Index)
Useful in diabetics where calcified arteries make ABI inaccurate.
5. Duplex Arterial Scan
Combines ultrasound + Doppler to identify the level and severity of block.
6. CT Angiography / MR Angiography
7. Digital Subtraction Angiography (DSA)
This is the Gold-standard vascular imaging test to detect exact blockages and plan angioplasty / stenting
Treatment of Peripheral Artery Disease (PAD) in Diabetics
Treatment aims to:
- Improve blood flow
- Prevent ulcers & gangrene
- Heal existing wounds
- Avoid amputation
- Improve walking ability
A comprehensive approach is required.
1. Lifestyle Modifications
- Quit smoking
- Regular exercise
- Weight control
- Diabetic diet plan
- Foot protection
These slow the progression of PAD.
2. Blood Sugar, Blood Pressure & Cholesterol Control
Strict control of HbA1c, LDL cholesterol, Blood pressure reduces further artery damage.
3. Medications
a. Antiplatelets: Aspirin and Clopidogrel prevent clot formation.
b. Cholesterol-lowering Drugs
Statins- Stabilize plaque and prevent further narrowing.
c. Vasodilators
Improve circulation and walking distance.
4. Foot & Wound Care in PAD
- Regular foot examination
- Treatment of calluses, corns, cracks
- Offloading pressure
- Infection control
- VAC dressing for ulcers
- Advanced wound therapies
PAD wounds require specialized diabetic foot care.
5. Angioplasty & Stenting (Endovascular Treatment)
a) Angioplasty: A balloon is inserted and inflated to open the blocked artery.
b) Stenting: A stent is placed to keep the artery open.
Benefits:
- Immediate blood flow improvement
- Faster healing of ulcers
- Prevents limb loss
- Short recovery time
6. Bypass Surgery for Severe PAD
For long or multiple blockages.
A vein or synthetic graft is used to create a new pathway for blood flow.
Indicated when:
- Angioplasty is not possible
- Multiple long-segment occlusions
- Critical limb ischemia with tissue loss
7. Amputation (Last Resort Only)
Done only when:
- Infection is spreading
- Gangrene is life-threatening
- Tissue is completely dead
Goal: protect life when the limb cannot be saved.
